Why Most Hospitals Are One Incident Away from a Serious Data Compliance Problem
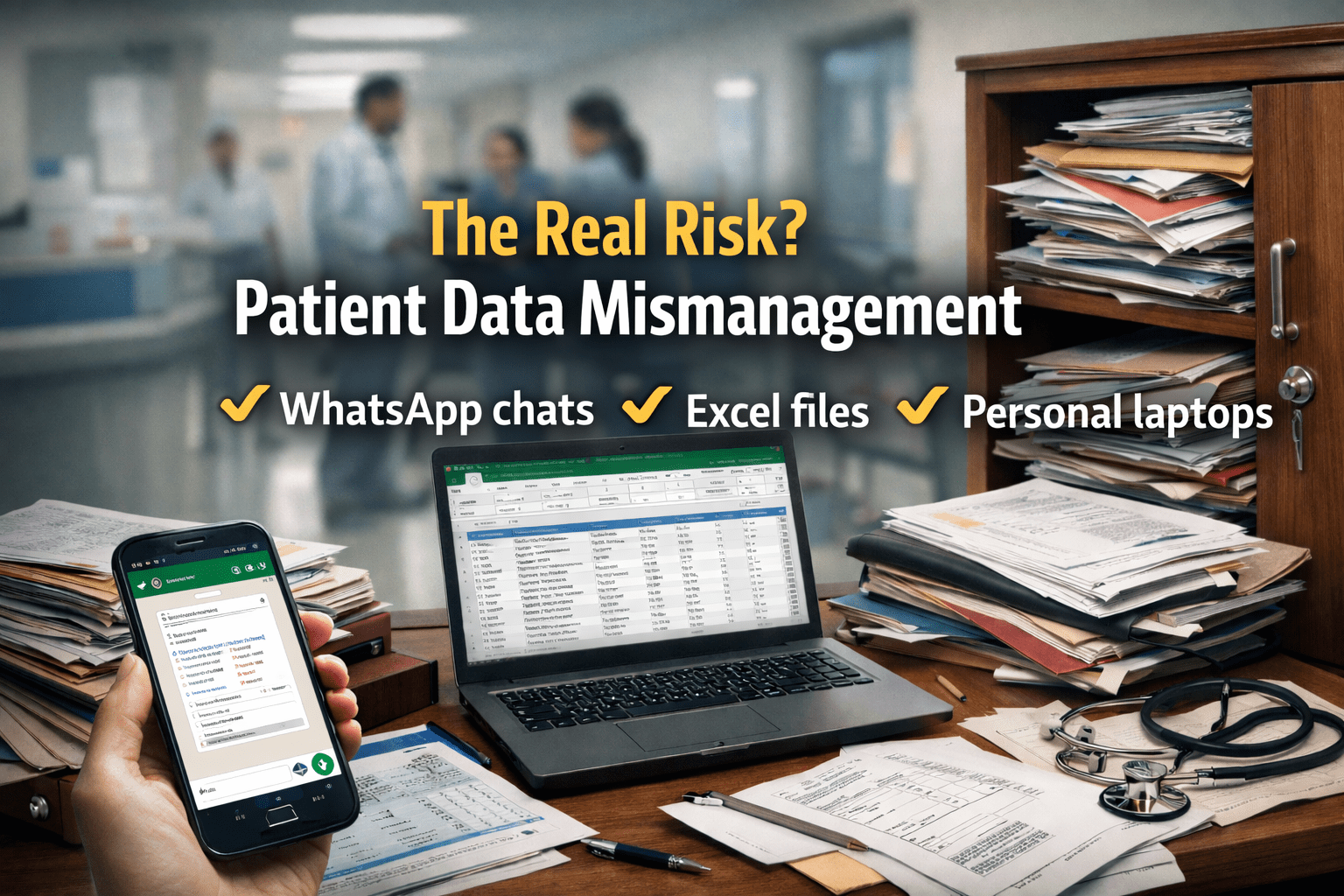
Most hospital leaders believe their biggest data risk is a cyberattack. That’s not true.
In small and mid-sized Indian hospitals, the real danger is far more ordinary and far more common. Patient data lives in Excel files, WhatsApp chats, personal laptops, email inboxes, and unlocked cupboards. Everyone knows this is not ideal. Almost no one treats it as urgent.
Until something goes wrong.
Patient data mismanagement rarely explodes overnight. It accumulates quietly through convenience-driven decisions, informal workarounds, and the assumption that healthcare is somehow exempt from the data discipline expected in other industries. That assumption no longer holds.
The Real Problem: Patient Data Is Everywhere and Owned by No One
In most hospitals, there is no single, controlled source of truth for patient information.
What actually happens on the ground:
- OPD details are entered in Excel for daily reporting.
- Lab reports are shared with patients and doctors over WhatsApp.
- Admission details are written on paper and later typed by billing.
- TPA documents are emailed back and forth without access control.
- Discharge summaries are saved on personal desktops “for convenience.”
Each step feels practical in isolation. Collectively, it creates a system where patient data is scattered, duplicated, and uncontrolled.
This persists because:
- Staff prioritise speed over structure.
- There is no clear data ownership.
- Leadership assumes “we’re not a target.”
- Compliance is seen as a paperwork exercise, not an operational one.
The result is not just inefficiency. It is risk,legal, financial, and reputational.
The Operational and Financial Impact of Patient Data Mismanagement
Compliance and Legal Exposure Under NABH and DPDP Act
Under NABH expectations, hospitals are required to maintain accurate, secure, and retrievable patient records. Fragmented data makes this difficult even on good days.
With India’s DPDP Act bringing sharper focus to data protection:
- Hospitals are clearly data custodians.
- Informal sharing and unsecured storage become liabilities.
- “We didn’t know” is not a defence.
When patient data is mishandled, hospitals face:
- Regulatory scrutiny
- Legal notices
- Loss of accreditation credibility
Financial Impact on Hospital Revenue and TPA Claims
Data mismanagement directly affects revenue:
- TPA claims are delayed or rejected due to missing or inconsistent documentation.
- Repeated follow-ups consume admin time.
- Disputes arise when records don’t align across departments.
These costs don’t appear as penalties at first. They appear as slower cash flow and rising administrative overhead.
Operational Impact on Hospital Staff and Daily Workflows
Staff spend time:
- Searching for old reports
- Reconfirming information already collected
- Re-entering data from paper to Excel to billing systems
The hospital becomes dependent on individuals “who know where things are.” When they are absent, work slows or stops.
Patient Trust
Patients increasingly expect privacy and professionalism. Casual handling of reports and personal details erodes confidence even if clinical care is strong.
Common Patient Data Governance Mistakes Hospitals Keep Making
- Using WhatsApp as a workflow tool
It is convenient, fast, and completely unmanaged. There is no access control, audit trail, or data retention policy. - Assuming Excel is harmless
Excel files are copied, emailed, renamed, and edited endlessly. No one knows which version is correct or who accessed it. - Letting staff use personal devices
Laptops and phones are not governed by hospital policy, yet they store sensitive patient data. - No access hierarchy
Everyone can see everything because “it’s easier.” This violates basic data governance principles. - Treating compliance as an annual event
Hospitals prepare for inspections, not for daily operational discipline.
These are not technical failures. They are governance failures.
What Actually Works in Real Hospitals
Hospitals that reduce data risk don’t rely on warnings or memos. They change how data flows.
What they do differently:
- Patient data is stored in one central system, not multiple tools.
- Access is role-based staff see only what they need.
- Data entry happens once and is reused across workflows.
- Sharing is controlled, traceable, and purposeful.
- Backups exist, and recovery is tested.
Importantly, these hospitals don’t slow down operations to achieve control. They remove the chaos that forces staff to create shortcuts in the first place.
How a Modern HMS Reduces Patient Data Risk
A modern Hospital Management System doesn’t “secure data” in theory. It makes insecure behaviour unnecessary.
Operationally, it:
- Eliminates the need for Excel and WhatsApp for core workflows
- Centralizes patient records with controlled access
- Maintains audit trails automatically
- Ensures data consistency across OPD, IPD, lab, pharmacy, and billing
- Makes records available instantly during audits or disputes
This is not about compliance checklists. It is about running a hospital where information is reliable, available, and protected by design.
When systems support staff properly, unsafe workarounds disappear on their own.
A Practical Data Compliance Self-Check for Hospital Leadership
Ask yourself honestly:
- Where does patient data live today everywhere, or somewhere controlled?
- Can you say who accessed a patient record last week?
- Are lab reports still being shared informally?
- Could you confidently explain your data handling practices during an inspection?
- If a staff member left tomorrow, would critical patient data leave with them?
If these questions make you uncomfortable, the risk already exists.
Final Thought: Patient Data Governance Is No Longer Optional
Patient data mismanagement is not a future problem. It is a current operational reality hiding in plain sight. Hospitals that ignore it are not avoiding complexity, they are postponing accountability.
The real question is not whether data governance matters, but whether your hospital is prepared to defend how it handles patient information when it’s finally questioned.
If you had to justify your data practices tomorrow to a regulator, a court, or a patient would you be confident, or scrambling?